www.know_the_risk_of_5fu_chemotherapy.com
ask about your risk of VERY serious side effects before starting 5-FU Chemotherapy
David's Story
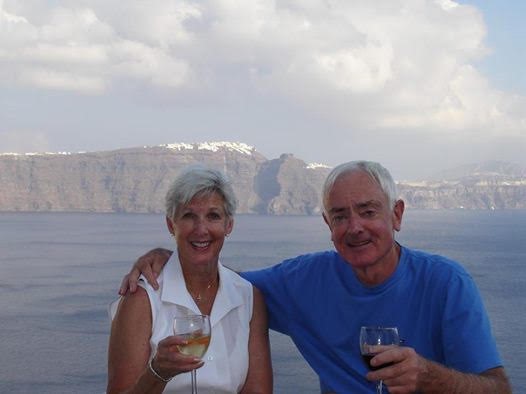
“David’s Story”
My husband of 51 years, David McIntyre, passed away on December 12, 2018, at Oregon Health and Science University Hospital in Portland, Oregon. David was diagnosed with Cholangiocarcinoma, Stage 1, in July of 2018. He had a successful Whipple surgery with clear margins, no metastasis and no lymph node involvement -- it was the best possible outcome. Despite some remaining pre-cancerous cells, he was nevertheless pronounced “cancer free” by his Radiation Oncologist. Radiation was not recommended. His oncologist, however, prescribed Capecitabine as adjuvant chemotherapy.
The Capecitabine literature David received from the oncologist, the hospital pharmacy and the manufacturer listed all of the usual and expected side-effects of the chemo, with only one line warning not to take Capecitabine if you had a “known DPD enzyme deficiency.” No symptoms for DPD enzyme deficiency reactions to Capecitabine were listed. The most serious side-effect discussed with us was Hand-Foot syndrome.
There was no mention that 1 in 1,000 people have the genetic DPD enzyme deficiency which could be fatal when taking Capecitabine, as it is needed to metabolize the chemo; a blood or saliva test to detect the DPD enzyme was not offered (not yet FDA mandated). David started the chemo with little concern, as we were told that it was generally well-tolerated and widely prescribed. We were not aware that about 1300 people die every year from undiagnosed DPD enzyme deficiency while taking 5-FU or capecitabine.
On the 7th day of his first round of chemo (the day after Thanksgiving), David began to experience vomiting and diarrhea. On Saturday, his symptoms increased to a few mouth blisters and the start of a rash on his face. I alerted his doctor with a voice message (office closed). I called the oncologist’s office on Monday, asking that David be seen, as his symptoms were worsening. I was advised by the nurse to have David take over-the-counter medications for the vomiting, diarrhea and rash. I asked her to alert the oncologist that I had called and was very concerned.
On Tuesday, I called the oncologist’s office again and reported that I was taking him to the ER, and asked that his doctor be alerted. His vomiting, diarrhea, mouth blisters, body rash and mucositis were continuing to worsen. He was kept in the ER overnight as an “observation” patient, treated for each of his symptoms, with a focus on the body rash, and sent home the next day, despite intractable diarrhea and ever worsening symptoms.
On Friday I called the doctor’s office again to report my concerns and was instructed to go to the hydration clinic on Saturday. The next day, Saturday, his temperature was 101 deg. and we went immediately to the ER. He was quickly admitted into the hospital because of severe neutropenia. He was seen by Interns and residents over the weekend, and yet not one of the doctors suspected DPD enzyme deficiency. It wasn’t until Monday morning that he was seen by an experienced oncologist making rounds that his symptoms were immediately recognized as DPD enzyme deficiency toxicity. We were told that an antidote, Vistogard, was being ordered but were not informed that there was a 96-hour window of reversal. By the time Vistogard was started through an NG feeding tube, he was already beyond that window by 6 days. It was too late to save his life, and yet we were encouraged by all the medical staff to remain optimistic that he would survive.
Had all of the medical staff (oncology nurses, ER staff and especially his oncologist) responded quickly and treated him appropriately as having a fully systemic, toxic breakdown indicative of a DPD enzyme deficiency, rather than treating each of his symptoms individually, there would have been time to order and administer the antidote within the critical 96-hour window following last chemo pill. His oncologist did not see him in person until a week following my first phone call, asking for help.
David died an excruciatingly painful death seven days following the start of Vistogard. He suffered three strokes, developed pneumonia, aspirated; his entire body was decimated, and he was essentially comatose the last 4 days of his life. Our family is devastated. And angry. And determined to spread the word about DPD enzyme deficiency and pre-testing prior to starting Capecitabine/Xeloda or 5-FU. In addition, I believe a more aggressive and comprehensive protocol by the oncology team (including nurses, ER staff and Pharmacist) needs to be in place to closely monitor patients’ tolerance of their chemotherapy, especially when DPD enzyme pre-testing is not offered. Given the current “Standard of Care” to NOT test for DPD enzyme deficiency, oncologists, I believe, are violating their Hippocratic Oath “…to do no harm.” . At the very least, the availability of Vistogard should have changed the “Standard of Care” protocols to allow for early recognition of this toxicity in time to administer the antidote. While we are waiting for the FDA to mandate testing, patients need to be informed of this potentially lethal outcome and oncologists have a duty and a responsibility to their patients to offer the test. It should not be up to the oncologists to play Russian roulette with their patients’ lives. Testing is now required by law in France, Italy and The Netherlands. With tests currently available to detect up to 90% of the genetic variables, it’s time for the US to get on board and start saving lives!